What is dry age-related macular degeneration?
Dry age-related macular degeneration (Dry AMD) is a common eye condition that affects people over the age of 50. It is a chronic condition that causes the cells in the retina to slowly deteriorate, leading to blurred or reduced central vision.
The term "dry" does not refer to dry eyes but rather to the fact that this condition is not the "wet" type of macular degeneration. About 85% of all cases of macular degeneration are Dry AMD, and 15% are wet or neovascular AMD.
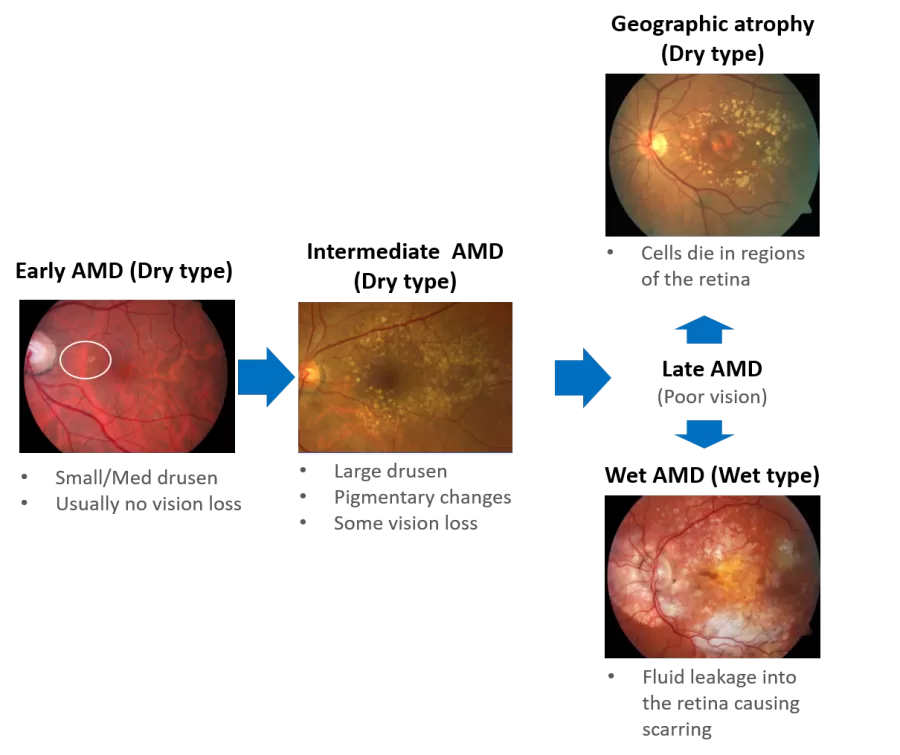
There are three stages of macular degeneration: early, intermediate, and late. In early dry AMD, there is little or no vision loss. In intermediate dry AMD, there may be some changes or loss of central vision, but the progression is slow. In late AMD, vision is severely impacted, and it is divided into the wet form or the dry form. And late dry AMD is also known as geographic atrophy or GA.
In geographic atrophy, the light-sensitive cells in the macula become thinner and eventually die in specific regions or spots, leading to areas of atrophy. This is why the condition is called geographic atrophy or atrophic AMD, as it resembles a map when the doctor examines the retina.
It's important to note that Dry AMD does not necessarily lead to complete blindness, although it can impact a person's ability to perform daily tasks, such as reading, driving, and recognizing faces. Legal blindness is commonly defined as 20/200 visual acuity, and people with legal blindness may still have some usable vision.
Did you know that Geographic atrophy has many synonyms, such as late/advanced dry AMD, atrophic AMD, end-stage dry AMD, late-stage non-neovascular AMD, or late nonexudative AMD?
What are the symptoms of dry AMD?
Your eye doctor may detect signs of dry AMD during a routine eye examination. These signs include drusen, small yellow deposits on the retina, and pigment changes in the macula. Dry AMD typically progresses slowly over time, so these signs may be present for a long time before you experience any vision-related symptoms.
The symptoms of dry AMD include:
Reduced central vision in one or both eyes
A well-defined blurry or blind spot in your field of vision (also called a scotoma)
Difficulty recognizing faces
Objects appear to change shape or size, and words become blurry or disappear when reading
The need for brighter light when reading or doing close-up work
Increased difficulty adapting when moving between light and dark rooms
Colors appearing faded
Straight lines appearing bent or distorted
Dry AMD may affect one or both eyes. If only one eye is affected, you may not notice any changes in your vision as your good eye compensates for the affected eye. Unlike wet AMD, it does not affect your peripheral vision, so it rarely leads to complete blindness.
Fun fact: The word "drusen" is German for "rock" or "geode" because they resemble small pebbles of debris under the retina.
What is the cause of dry age-related macular degeneration?
The exact cause of dry AMD is still unknown, but research indicates that a combination of heredity and environmental factors such as smoking, obesity, and diet may play a role. Recent research has further shed light on the role of the complement pathway in the development and progression of dry AMD.
The complement pathway is part of the immune system that helps protect the body against harmful intruders, such as germs and viruses. When the complement cascade is triggered, it creates pieces that can kill these intruders but also retina cells, leading to vision loss. One of these pieces, called C3, splits into two smaller pieces, C3a and C3b. Another piece, called C5, splits into C5a and C5b. These pieces can combine to form inflammasome and membrane attack complex (MAC) structures that cause cell damage.
In the early stages of the condition, small deposits called drusen may be visible in the back of the eye. As the disease progresses, the drusen become larger and more numerous, and changes in the retina pigment become noticeable. In the late stage, an advanced form of dry AMD called geographic atrophy develops, causing large areas of retina cells to die off and creating permanent blind spots in the visual field.
What are the risk factors for dry AMD?
Some factors that may increase your risk of developing dry AMD include:
Age: People over 55 years old, with a higher risk for those over 75.
Family history: A family history of AMD increases your risk of developing the condition.
Ethnicity: Being of Caucasian descent is a risk factor.
Gender: Women have a higher risk of developing AMD compared to men.
Smoking: Smoking is a significant risk factor for AMD.
Cardiovascular disease: Having cardiovascular disease increases your risk of developing AMD.
Obesity: Research suggests that obesity may increase the progression of early-stage AMD to the more severe wet form of AMD.
How is dry AMD diagnosed?
During your appointment with your eye doctor, they will begin by discussing your health history and any previous vision problems you or your family may have experienced. This information will help the doctor to better understand any potential risk factors for eye conditions. The eye doctor will then proceed with a comprehensive eye exam. It may include:
Retina examination: Your eye doctor will dilate your eyes and use a special instrument to examine the back of your eye and identify yellow spots.
Visual field testing: An Amsler grid is used to test your vision. If you have macular degeneration, some straight lines in the chart may look faded, broken, or distorted.
Fundus photography: This is a non-invasive imaging technique that allows the optometrist to take detailed photographs of the retina and macula. The images can be enhanced and can reveal changes or damage to the macula, which could be indicative of macular degeneration.
Optical coherence tomography (OCT): This imaging test provides detailed cross-sectional images of the retina and identifies areas of retina thinning, thickening, or swelling caused by fluid accumulation from leaking blood vessels.
Other tests that your doctor may also do if they suspect you also have abnormal blood vessel growth:
Fluorescein angiography: This test is performed if your doctor suspects abnormal blood vessel growth under the retina. A fluorescein dye is injected into a vein in your arm and highlights the blood vessels in the eyes, with a special camera taking pictures of any leakage as the dye travels through the vessels.
Indocyanine green angiography: Like fluorescein angiography, this test is performed if your doctor suspects abnormal blood vessel growth under the retina. It uses an injected dye called indocyanine green to identify specific types of macular degeneration.
How fast does AMD progress?
The progression of early and intermediate AMD is usually slow and may take years, but this can vary from person to person. For example, within 5 years, up to 3 out of 100 people with early AMD may progress to intermediate AMD, while half of those with intermediate AMD may advance to the late stage. This means about 15% of people with early AMD may progress to the late stage in 10 years.
If a person has large drusen in both eyes, their risk of developing late AMD within five years increases to 26%. And if a person has late AMD in one eye, their risk of also developing to a late stage in the other eye is between 35-50%.
I have been diagnosed with age-related macular degeneration. What should I do?
If you have been diagnosed with Age-related Macular Degeneration (AMD), it is important to take steps to manage your condition and maintain your vision. While there is currently no cure for dry AMD, there are steps you can take to slow down its progression.
Educate yourself: Understanding your condition is the first step in managing it. Many people with dry AMD are able to maintain good vision for the rest of their lives.
Consult your doctor: Your doctor is the best person to answer any questions you may have about your condition and discuss supplement and treatment options. Regular eye exams are crucial in monitoring the progression of your condition, and your doctor may recommend appointments every month for late AMD or every few months, depending on your diagnosis.
Monitor for progression: Use an Amsler grid, a common home screening tool, to check for any signs of progression in your vision. You can find an Amsler grid here.
Reduce your risks: Take steps to reduce the risk of progression, such as eating a healthy diet, quitting smoking, and wearing protective eyewear.
By taking these steps, you can help prevent dry AMD from worsening.
How to prevent early dry AMD from worsening?
If you are at high risk of developing dry AMD or if you are diagnosed with early or intermediate AMD, you can take steps to reduce your risk or slow its progression:
Quit smoking: If you smoke, quitting smoking can greatly reduce your risk of developing macular degeneration. Ask your doctor about smoking cessation programs near you.
Manage cardiometabolic conditions: Conditions such as hypertension, hyperlipidemia, or diabetes can increase your risk of macular degeneration. Follow your doctor's instructions for controlling these conditions.
Maintain a healthy weight and exercise: Being obese increases the risk of macular degeneration progressing to a more severe form. Maintain a healthy weight and exercise regularly.
Healthy diet: Choose a diet rich in fruits and vegetables, and include foods high in omega-3 fatty acids, such as fish (salmon, tuna, and mackerel) and nuts (such as walnuts, peanut, and hazelnut).
Vitamin supplements: Ask your doctor about taking vitamin and mineral supplements, such as the AREDS2, to reduce your risk of developing AMD. (More on AREDS2 supplement)
Note: It is important to consult with your doctor before making any changes to your diet or taking any new supplements.
How to treat dry AMD?
If you have dry age-related macular degeneration (AMD) with geographic atrophy (GA), a new treatment option is now available. On February 17, 2023, the FDA approved SYFOVRE (pegcetacoplan injection) to treat GA in people with AMD. This is the first drug approved by the FDA for this condition.
SYFOVRE works by blocking the action of proteins that contribute to the growth of GA. The treatment is given as an eye injection, usually every 25 to 60 days. Clinical trials have shown that SYFOVRE can reduce the growth of GA better than a sham (didn’t receive the drug treatment). And the improvement was seen to increase over time.
Like all treatments, SYFOVRE can cause side effects. The most common side effects include discomfort, increased risk of developing wet AMD, floaters in vision, and bleeding in the white part of the eye.
SYFOVRE will be available in the US starting in March 2023. If you have dry AMD and are interested in learning more about this new treatment, talk to your eye doctor. They can help you understand if SYFOVRE is right for you and explain the potential benefits and risks.
(Learn more about SYFOVRE and upcoming treatments for geographic atropine)
Are there vitamin supplements for dry age-related macular degeneration?
If you have dry AMD, you may have heard that there are supplements that can help. Research has been done on what supplements can slow down the progression of AMD. According to the National Eye Institute, a specific combination of supplements called AREDS2 was shown in a study to slow down the worsening of dry AMD.
The AREDS2 supplement may be able to stop the progression of intermediate AMD in one or both eyes into late AMD. If you have late AMD in only one eye, it may also slow down the progression in the other eye. However, if you already have late AMD in both eyes, taking the AREDS2 supplement is unlikely to be of benefit.
The AREDS2 nutrient formula contains the following ingredients: Vitamin C (500mg), Vitamin E (400 IU), Copper (2mg), Lutein (10mg), Zeaxanthin (2mg), and Zinc (80mg).
While taking supplements may be helpful for some people, it's important to be aware that there may also be health risks. Discuss with your doctor before taking any new supplements to determine if they are appropriate for you.
(Learn more about the benefits, risks, and recommended daily intake of different vitamins)